They say there is no rehearsal for life but there is at The Dr. James W. Mounsey Clinical Simulation Lab at Sacred Heart Medical Center.
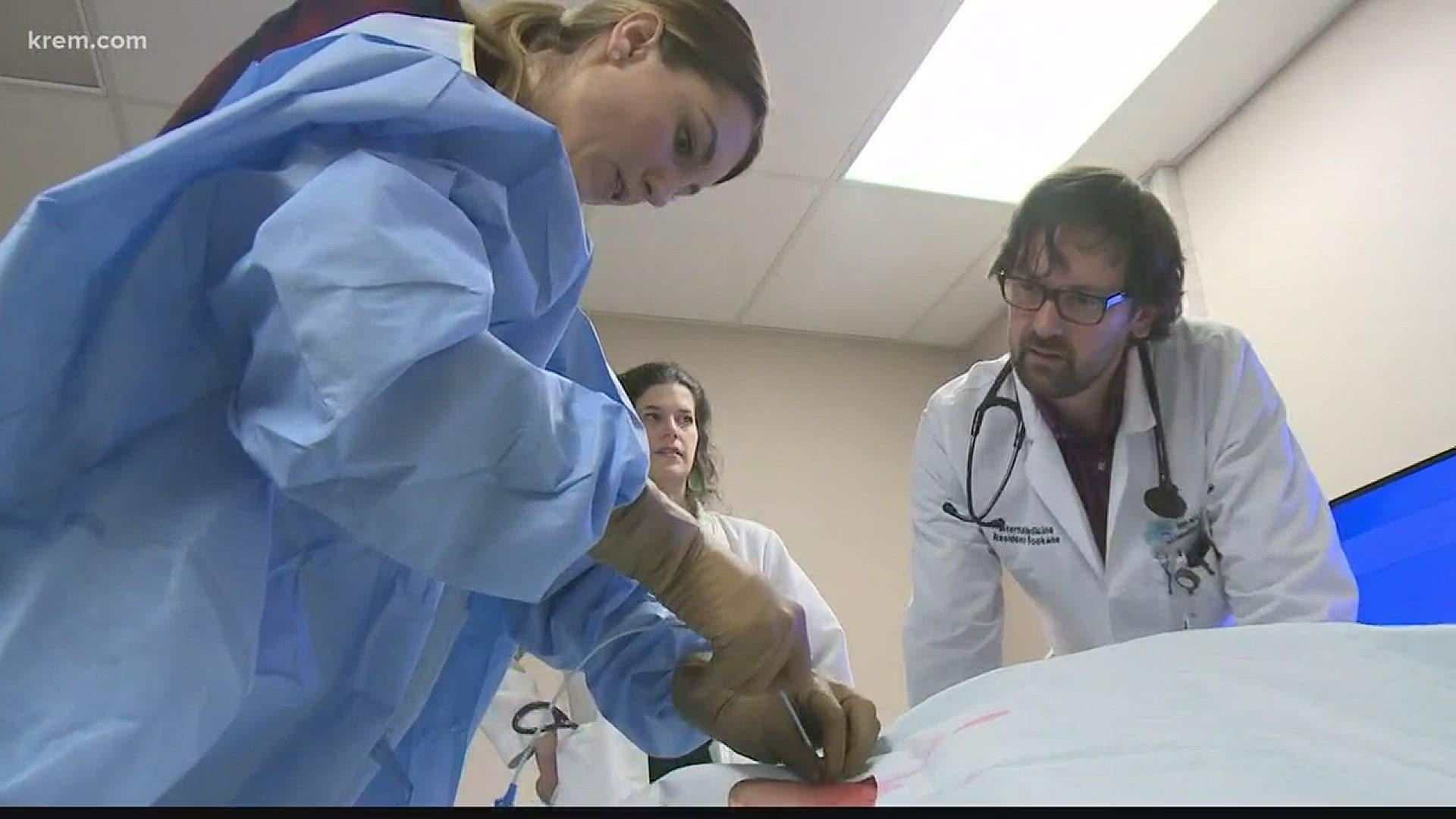
Current and future medical professionals like Resident Physician Lucy Ledyard practice their technical skills on robotic patients before treating human patients.
After receiving a generous donation from the Mounsey family Sacred Heart Medical Center converted the same day surgery center into a simulated ICU and OR. A flexible space fit to educate staff and students.
Doctor James Mounsey, the namesake for the simulation lab, was one of the first medical residents to go through sacred heart in 1919 and 1920. He became a well-known surgeon in the area. According to his family, he was a devout Catholic and would provide free medical care to the poor.
“The family tells stories of lines going out of the building being halfway down the block waiting for an appointment with him. They wanted to carry on the legacy of their grandfather,” said lab director and registered respiratory therapist Wade Scoles.
Once a month physicians - including internal medical specialist doctor Amy Eddy and clinical coordinator Wade Scoles - create real-life, hands-on, high- pressure patient scenarios using mannequins to train current and new hospital staff.
“We go over how to run a code, how to place a central line and how to use the ultrasound to identify vessels and access them, go over other procedures such as arterial line placement and thoracentesis and paracentesis so when they are in the thick of it, they have done it before,” said Eddy.
Practitioners are not only learning clinical skills. Away from the high-risk environment of actual patient care, this “no-risk” laboratory increases proficiency, builds confidence and enhances teamwork.
“In addition to the procedural skills that we practice we also practice communication skills and how to communicate in a team in an especially stressful manner to make sure there is leadership and the least amount of miscommunication,” said Eddy.
Ledyard is practicing her skills and preparing for her upcoming ICU rotation. She is learning how to place a central venous catheter into a life like dummy that bleeds and can communicate like a human-being.
“The mannequins breathe, bleed, cough and otherwise simulate just about everything a real human patient would, “said Scoles.
Placement of a central line, the long flexible tube used to give medications, fluids, nutrients over long periods of time is a routine procedure but can be difficult for new clinicians in an emergent situation.
“In a real-life situation, you’re getting that line in and you are worried about things like bleeding and the time of it, whereas here we can stop and adjust half way through to make sure we are getting the techniques right,” said Ledyard.
Physician technique can affect patient care. A study by researchers at Johns Hopkins Medicine says more than 250,000 Americans die each year from medical that range from surgical complications that go unrecognized to mix-ups with the doses or types of medications patients receive. The main goal of the Simulation Center is to improve safety within patient care
“Because these are usually under stressful circumstances and that some of them are fairly high risk, and we absolutely cannot be wrong that it helps to have them have some training wheels even though it is not exactly like real life so that when they do it they have a better chance at success,” said doctor Eddy.
The best way to learn is by doing. But in medicine, that can be risky when a new graduate has to jump into a complex case.
“Historically medicine has been see one do one teach one and I think that is not the best for our learners and certainly not the best for our patients, “stressed doctor Eddy
All of the “robotic patients” are named, kept warm and treated like human patients.
“We never want to lose site of the fact that every mannequin here represents human life. Good performance, saving a mannequin here can absolutely translate into saving the life of a human,” said Scoles
Before the simulation lab opened, Ledyard only had the opportunity to observe in the past. Now she feels more confident treating patients.
“Once you get into the ICU there is such a high stress environment that being able to do it here and just knowing the steps and the mechanics in a very controlled very low stress environment, I think will make the day very easy when I get to the ICU and have to do it,” shared Ledyard.
After this ICU rotation, doctor Ledyard will relocate to Vermont to complete her training and dermatology residency over the next three years
Not only is the simulation lab a creative environment for professionals to learn, they will soon be opening their doors to teach middle and high-school students about the different careers and opportunities available in healthcare.
“In October, this year we trained over 300 people in the SIM Lab,” Scoles said. “It’s the busiest month to date and it’s just the beginning. We are getting busier and busier.”